🫀 Heart Structure
Key Concept
The heart is a muscular pump that maintains blood circulation throughout the body. It consists of four chambers and is divided into left and right sides, each with specific functions.
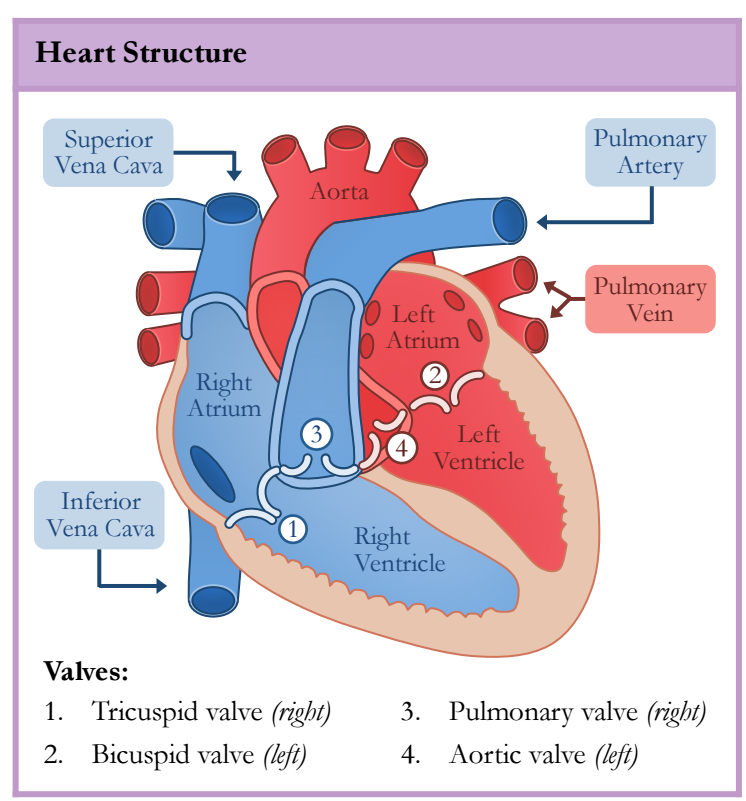
Figure 1: Structure of the human heart showing chambers, valves, and major blood vessels
Four Chambers of the Heart
Right Side (Deoxygenated Blood)
- Right Atrium: Receives deoxygenated blood from the body via the superior and inferior vena cava
- Right Ventricle: Pumps deoxygenated blood to the lungs via the pulmonary artery
Left Side (Oxygenated Blood)
- Left Atrium: Receives oxygenated blood from the lungs via the pulmonary vein
- Left Ventricle: Pumps oxygenated blood to the body via the aorta
The left ventricle has a thicker muscular wall than the right ventricle because it must generate enough pressure to pump blood throughout the entire body, while the right ventricle only pumps blood to the nearby lungs.
Heart Valves
The heart contains four valves that prevent backflow of blood and ensure unidirectional flow:
| Valve | Location | Function |
|---|---|---|
| 1. Tricuspid Valve | Between right atrium and right ventricle | Prevents backflow from right ventricle to right atrium |
| 2. Bicuspid Valve (Mitral) | Between left atrium and left ventricle | Prevents backflow from left ventricle to left atrium |
| 3. Pulmonary Valve | Between right ventricle and pulmonary artery | Prevents backflow from pulmonary artery to right ventricle |
| 4. Aortic Valve | Between left ventricle and aorta | Prevents backflow from aorta to left ventricle |
Major Blood Vessels
- Superior & Inferior Vena Cava: Bring deoxygenated blood from the body to the right atrium
- Pulmonary Artery: Carries deoxygenated blood from the right ventricle to the lungs
- Pulmonary Vein: Brings oxygenated blood from the lungs to the left atrium
- Aorta: Carries oxygenated blood from the left ventricle to the body
The pulmonary artery carries deoxygenated blood (even though it's an artery), and the pulmonary vein carries oxygenated blood (even though it's a vein). Remember: arteries carry blood AWAY from the heart, veins carry blood TO the heart!
🔄 Blood Flow Through the Heart
Pathway of Blood Circulation
Blood follows a specific pathway through the heart in a double circulation system: pulmonary circulation (heart → lungs → heart) and systemic circulation (heart → body → heart).
Step-by-Step Blood Flow
🔵 Deoxygenated Blood Pathway (Right Side)
- Deoxygenated blood from the body enters the right atrium via the superior and inferior vena cava
- Blood flows through the tricuspid valve into the right ventricle
- The right ventricle contracts, pushing blood through the pulmonary valve
- Blood travels via the pulmonary artery to the lungs for oxygenation
🔴 Oxygenated Blood Pathway (Left Side)
- Oxygenated blood from the lungs enters the left atrium via the pulmonary vein
- Blood flows through the bicuspid (mitral) valve into the left ventricle
- The left ventricle contracts powerfully, pushing blood through the aortic valve
- Blood travels via the aorta to supply the entire body with oxygen and nutrients
The double circulation system allows blood to be pumped to the lungs at lower pressure (preventing damage to delicate lung tissue) while maintaining high pressure for systemic circulation to reach all body tissues efficiently.
Interactive Blood Flow Visualization
💓 The Cardiac Cycle
Definition
The cardiac cycle is the sequence of events that occurs during one complete heartbeat, consisting of systole (contraction) and diastole (relaxation).
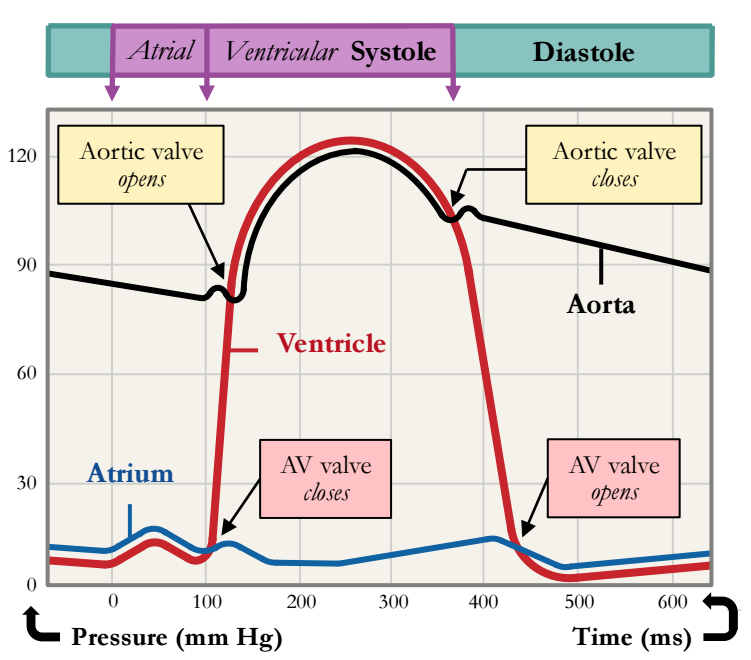
Figure 2: Pressure changes in the atrium, ventricle, and aorta during the cardiac cycle
Phases of the Cardiac Cycle
1️⃣ Atrial Systole
- Atria contract
- AV valves (tricuspid & bicuspid) open
- Blood pushed into ventricles
- Ventricles fill completely
2️⃣ Ventricular Systole
- Ventricles contract
- AV valves close (prevents backflow)
- Semilunar valves (pulmonary & aortic) open
- Blood ejected to lungs and body
3️⃣ Diastole (Relaxation Phase)
- All chambers relax
- Semilunar valves close (prevents backflow from arteries)
- AV valves open
- Blood flows passively from atria to ventricles
- Heart refills with blood
Pressure Changes During the Cardiac Cycle
- Atrial pressure remains relatively low throughout the cycle
- Ventricular pressure rises sharply during ventricular systole (up to ~120 mm Hg)
- Aortic pressure rises when the aortic valve opens and blood is ejected
- Valve opening and closing is determined by pressure differences between chambers
Heart Sounds: "Lub-Dub"
| Sound | Cause | Timing |
|---|---|---|
| "Lub" (S1) | Closure of AV valves (tricuspid & bicuspid) | Start of ventricular systole |
| "Dub" (S2) | Closure of semilunar valves (pulmonary & aortic) | Start of diastole |
Interactive Cardiac Cycle Simulation
⚡ Control of Heart Rate
Myogenic Muscle
The heart is myogenic, meaning it can contract and relax without receiving signals from the nervous system. The heartbeat is initiated by the heart's own pacemaker cells.
The Sinoatrial Node (SAN) - Natural Pacemaker
Function: Generates electrical impulses that set the rhythm of the heartbeat
Rate: Approximately 60-100 beats per minute at rest
Pathway of Electrical Conduction
- Sinoatrial Node (SAN) generates an electrical impulse
- Impulse spreads across both atria, causing them to contract (atrial systole)
- Impulse reaches the Atrioventricular Node (AVN) at the base of the right atrium
- AVN delays the signal briefly (allowing atria to finish contracting)
- Impulse travels down the Bundle of His in the septum
- Signal spreads through Purkinje fibers in the ventricle walls
- Ventricles contract from the bottom up (ventricular systole)
If the SAN fails, the AVN can take over as a backup pacemaker, but at a slower rate (~40-60 bpm). Artificial pacemakers can be implanted to regulate heart rhythm in cases of severe dysfunction.
Regulation of Heart Rate
While the heart is myogenic, the autonomic nervous system can modify the heart rate:
⬆️ Sympathetic Nervous System
- Releases epinephrine (adrenaline)
- Increases heart rate
- Increases force of contraction
- Active during exercise or stress
⬇️ Parasympathetic Nervous System
- Releases acetylcholine
- Decreases heart rate
- Active during rest and relaxation
- Helps conserve energy
$\text{Cardiac Output} = \text{Heart Rate} \times \text{Stroke Volume}$
🩺 Coronary Heart Disease (CHD)
Definition
Coronary Heart Disease (CHD) occurs when the coronary arteries that supply the heart muscle with oxygen and nutrients become narrowed or blocked, typically due to atherosclerosis.
Atherosclerosis: The Underlying Cause
What is Atherosclerosis?
Atherosclerosis is the buildup of fatty deposits (plaques) on the inner walls of arteries, leading to:
- Narrowing of the artery lumen (stenosis)
- Reduced blood flow to the heart muscle
- Decreased oxygen delivery (ischemia)
- Potential for complete blockage (thrombosis)
Progression of CHD
- Endothelial Damage: Inner lining of coronary arteries is damaged (by high blood pressure, smoking, high cholesterol)
- Lipid Accumulation: Low-density lipoproteins (LDL) accumulate in the artery wall
- Plaque Formation: White blood cells (macrophages) engulf lipids, forming foam cells and fatty streaks
- Plaque Growth: Smooth muscle cells proliferate, and calcium deposits form, creating a hard plaque
- Stenosis: Artery lumen narrows significantly, restricting blood flow
- Thrombosis: Plaque may rupture, triggering blood clot formation that can completely block the artery
Consequences of CHD
💔 Angina
Chest pain caused by reduced blood flow to the heart muscle, especially during physical exertion.
- Temporary oxygen shortage
- Relieved by rest
- Warning sign of CHD
🚨 Myocardial Infarction (Heart Attack)
Death of heart muscle tissue due to complete blockage of a coronary artery.
- Permanent damage
- Medical emergency
- Can be fatal
- Severe chest pain (crushing sensation)
- Pain radiating to left arm, neck, or jaw
- Shortness of breath
- Nausea and sweating
- Anxiety and sense of impending doom
Treatment Options
| Treatment | Description | Purpose |
|---|---|---|
| Medications | Statins, antiplatelet drugs, beta-blockers | Lower cholesterol, prevent clots, reduce heart workload |
| Angioplasty | Balloon catheter inserted to widen artery | Restore blood flow |
| Stent Placement | Mesh tube inserted to keep artery open | Maintain blood flow long-term |
| Coronary Bypass Surgery | Vein/artery grafted to bypass blockage | Create alternative blood flow pathway |
⚠️ Risk Factors for Coronary Heart Disease
Understanding Risk
Risk factors are characteristics or behaviors that increase the likelihood of developing CHD. Some are modifiable (can be changed), while others are non-modifiable (cannot be changed).
Figure 3: Major risk factors for coronary heart disease (Mnemonic: GO DDES S)
Modifiable Risk Factors (Can Be Changed)
🍔 Obesity
Excess body weight, especially abdominal fat
- Increases blood pressure
- Raises cholesterol levels
- Linked to diabetes
- Solution: Maintain healthy weight through diet and exercise
🍟 Diet (High Trans Fats)
Consumption of saturated and trans fats
- Increases LDL cholesterol
- Promotes plaque formation
- Found in fried foods, processed foods
- Solution: Eat more fruits, vegetables, whole grains, lean proteins
🏃 Exercise (Inactivity)
Sedentary lifestyle
- Weakens heart muscle
- Reduces cardiovascular fitness
- Contributes to obesity
- Solution: At least 150 minutes of moderate exercise per week
🚬 Smoking
Tobacco use
- Damages artery walls
- Increases blood pressure
- Promotes blood clot formation
- Solution: Quit smoking immediately
Non-Modifiable Risk Factors (Cannot Be Changed)
🧬 Genetics
Family history of heart disease
- Inherited predisposition
- May include genetic high cholesterol
- Hypertension can run in families
- Action: Regular screening and preventive measures
👨 Sex (Male)
Males have higher risk
- Men develop CHD earlier than women
- Estrogen provides some protection in women
- Risk equalizes after menopause
- Action: Be aware and take preventive measures
Associated Medical Conditions
🩺 Diseases (Diabetes, Hypertension)
- Diabetes: High blood sugar damages blood vessels and nerves
- Hypertension (High Blood Pressure): Puts extra strain on artery walls, promoting atherosclerosis
- High Cholesterol: Excess LDL leads to plaque buildup
- Action: Manage these conditions through medication and lifestyle changes
- Genetics
- Obesity
- Diseases (diabetes, hypertension)
- Diet (high trans fats)
- Exercise (inactivity)
- Smoking
- Sex (male)
Risk Reduction Strategies
🥗 Dietary Modifications
- Reduce saturated and trans fats
- Increase omega-3 fatty acids (fish, nuts)
- Eat more fruits and vegetables (antioxidants)
- Choose whole grains over refined carbohydrates
- Limit salt intake to reduce blood pressure
🏋️ Exercise and Physical Activity
- Aim for 150 minutes of moderate aerobic activity per week
- Include strength training 2+ days per week
- Start slowly and gradually increase intensity
- Find activities you enjoy to maintain consistency
💊 Medical Management
- Regular health screenings (blood pressure, cholesterol, blood sugar)
- Take prescribed medications as directed
- Monitor and manage chronic conditions
- Consult healthcare providers regularly
Interactive Risk Assessment
📝 IB-Style Exam Questions
Question 1: Explain why the left ventricle has a thicker wall than the right ventricle. [3 marks]
Model Answer:
- The left ventricle must pump blood to the entire body / systemic circulation [1 mark]
- This requires generating much higher pressure than pumping to the lungs [1 mark]
- The thicker muscular wall allows for more powerful contractions to generate this pressure [1 mark]
Note: The right ventricle only pumps blood to the nearby lungs (pulmonary circulation), which requires lower pressure.
Question 2: Describe the pathway of blood through the heart, starting from the vena cava. [6 marks]
Model Answer:
- Deoxygenated blood enters the right atrium from the vena cava [1 mark]
- Blood flows through the tricuspid valve into the right ventricle [1 mark]
- Right ventricle contracts, pushing blood through the pulmonary valve into the pulmonary artery [1 mark]
- Blood travels to the lungs for gas exchange, then returns via the pulmonary vein to the left atrium [1 mark]
- Blood flows through the bicuspid (mitral) valve into the left ventricle [1 mark]
- Left ventricle contracts, pushing blood through the aortic valve into the aorta and to the body [1 mark]
Question 3: Explain how atherosclerosis can lead to a heart attack. [4 marks]
Model Answer:
- Atherosclerosis is the buildup of fatty deposits (plaques) in the coronary arteries [1 mark]
- This narrows the artery lumen, reducing blood flow to the heart muscle [1 mark]
- The plaque may rupture, triggering blood clot (thrombus) formation [1 mark]
- Complete blockage prevents oxygen delivery, causing heart muscle cells to die (myocardial infarction) [1 mark]
Question 4: Outline how the heart rate is controlled by the sinoatrial node (SAN). [3 marks]
Model Answer:
- The SAN is located in the wall of the right atrium and acts as the heart's natural pacemaker [1 mark]
- It generates electrical impulses that spread across the atria, causing them to contract [1 mark]
- The impulse is then transmitted to the ventricles via the AVN and Bundle of His, coordinating the heartbeat [1 mark]
Additional: The heart rate can be modified by the autonomic nervous system (sympathetic increases rate, parasympathetic decreases rate).
Question 5: Distinguish between modifiable and non-modifiable risk factors for coronary heart disease, giving two examples of each. [4 marks]
Model Answer:
Modifiable risk factors are those that can be changed through lifestyle modifications or medical intervention [1 mark]
Examples: Smoking, obesity, lack of exercise, high-fat diet [1 mark for two examples]
Non-modifiable risk factors are those that cannot be changed [1 mark]
Examples: Genetics/family history, sex (male), age [1 mark for two examples]